If you’re middle-aged or older, you may have noticed you’re experiencing more aches and pains than you used to.
What was once a little soreness after a pickup game of basketball or racquetball has turned into a lingering ache that never goes away. Is it osteoarthritis? Or is it normal aging aches and pains?
In this post, we’ll talk about how to tell the difference between osteoarthritis and age-related pain, what exactly osteoarthritis is, and how to prevent and treat it.
Why It’s Important to Identify Osteoarthritis Pain
Osteoarthritis, sometimes called OA, is the most common form of arthritis. As we age, most of us notice an increase in aches and pains in our bodies. But osteoarthritis isn’t just aches and pains. It’s a progressive, degenerative disease that eventually results in joint failure.
Because of the progressive nature of the disease, identifying and treating osteoarthritis early can make a major difference in your health outcomes. Modern interventions can markedly slow the degenerative process, and sometimes halt it altogether.
What Is Osteoarthritis?
Think of osteoarthritis as the wear and tear on a joint over time. The cushion of cartilage that covers the ends of the bones in a joint becomes damaged and wears down, resulting in bone-on-bone pain.
Osteoarthritis typically affects those middle-aged and older after years of joint overuse or abuse, though genetic predisposition can play a role, too.
Age-related pain, on the other hand, typically stems from the soft tissues surrounding a joint. Soreness and aches from “getting old” often come from tight or weakened muscles, lack of flexibility, loss of range of motion, and longer recovery times. But none of these issues indicate a problem within the joint itself.
How to Tell the Difference Between Osteoarthritis and Regular Aging
Because the symptoms and progression of osteoarthritis can vary quite a bit among individuals, people can have trouble identifying whether their pain is from OA, especially in the early stages. However, there are a few signs to watch for.
Pain duration. Osteoarthritis pain increases with use. The more you use an affected joint, the worse the pain gets. You’ll probably notice that osteoarthritis pain worsens as the day goes on but gets better with rest.
Age-related pains, on the other hand, often don’t wax and wane the same way osteoarthritis pain does. They may hurt regardless of how much you’re moving or resting.
Warmth, redness, and swelling. You may notice warmth or swelling around a joint with osteoarthritis, or it may appear red. These symptoms don’t always occur, especially around deeper joints like the hip, but if they do, they’re a helpful signpost. Normal aging shouldn’t cause any of these symptoms.
Imaging. Fortunately, you don’t need complicated or extensive testing to diagnose osteoarthritis. It shows up on a simple X-ray, sometimes even when no symptoms are present.
Strategies to Prevent Osteoarthritis
One of the biggest steps you can take to prevent osteoarthritis is to keep the muscles and tendons around your joints flexible and strong. When these stabilizing muscles and tendons become weak and inflexible, joints suffer more of the wear and tear that leads to OA.
Strengthen and stretch. To avoid knee osteoarthritis, for example, pay special attention to keeping your quadriceps muscles strong, and maintaining good flexibility and range of motion.
Avoid injury. If you aren’t used to exercising, start slowly to avoid hurting yourself. Be sure to seek treatment promptly if you suffer any joint injury.
Practice caution. To prevent osteoarthritis in the hands, take care when lifting, pushing, or pulling heavy objects, especially if you perform these tasks repeatedly. If you spend a lot of time typing on the computer, practice good posture and take plenty of breaks to rest and stretch your wrists, hands, and fingers.
Maintain a healthy weight. Maintaining a healthy weight can also help prevent osteoarthritis by reducing strain on weight-bearing joints. Diabetes, a disease often associated with weight gain, can also increase your risk of OA.
Techniques to Slow Osteoarthritis Progression
If you already have osteoarthritis, you can still make a difference in your joint health and pain level.
Strengthen and stretch. The first technique for preserving or restoring range of motion is similar to the first step in prevention: stretching and strengthening the muscles surrounding the joint. Again, remember to take this slowly. Pushing yourself too far will only make the osteoarthritis worse.
Anti-inflammatory drugs. Medications called NSAIDs (nonsteroidal anti-inflammatory drugs) can help manage the pain and swelling caused by osteoarthritis, especially in early stages. The most common NSAIDs are ibuprofen (Motrin, Advil), naproxen (Aleve), and diclofenac (Voltaren). Tylenol can also help manage pain, though it won’t ease swelling.
Joint injections. Joint injections are the next step for longer-term relief of serious osteoarthritis pain. Corticosteroid injections are the most common type of joint injection and decrease pain and swelling in the knee. Other types of joint injections use hyaluronic acid, platelet-rich plasma, or stem cells.
Joint replacement. Once a joint’s cartilage totally wears away, the only true cure for the bone-on-bone pain is joint replacement surgery. After the failed joint is replaced with artificial materials, the pain goes away immediately. Joint replacements have some risks, so talk to your doctor to see if joint replacement is right for you.
What to Do if You Suspect You Have Osteoarthritis
If you’ve been experiencing pain, redness, heat, and/or swelling in your joints, it’s important to talk to your doctor. If they suspect osteoarthritis, they’ll often order an X-ray sooner than they would for other injuries or conditions.
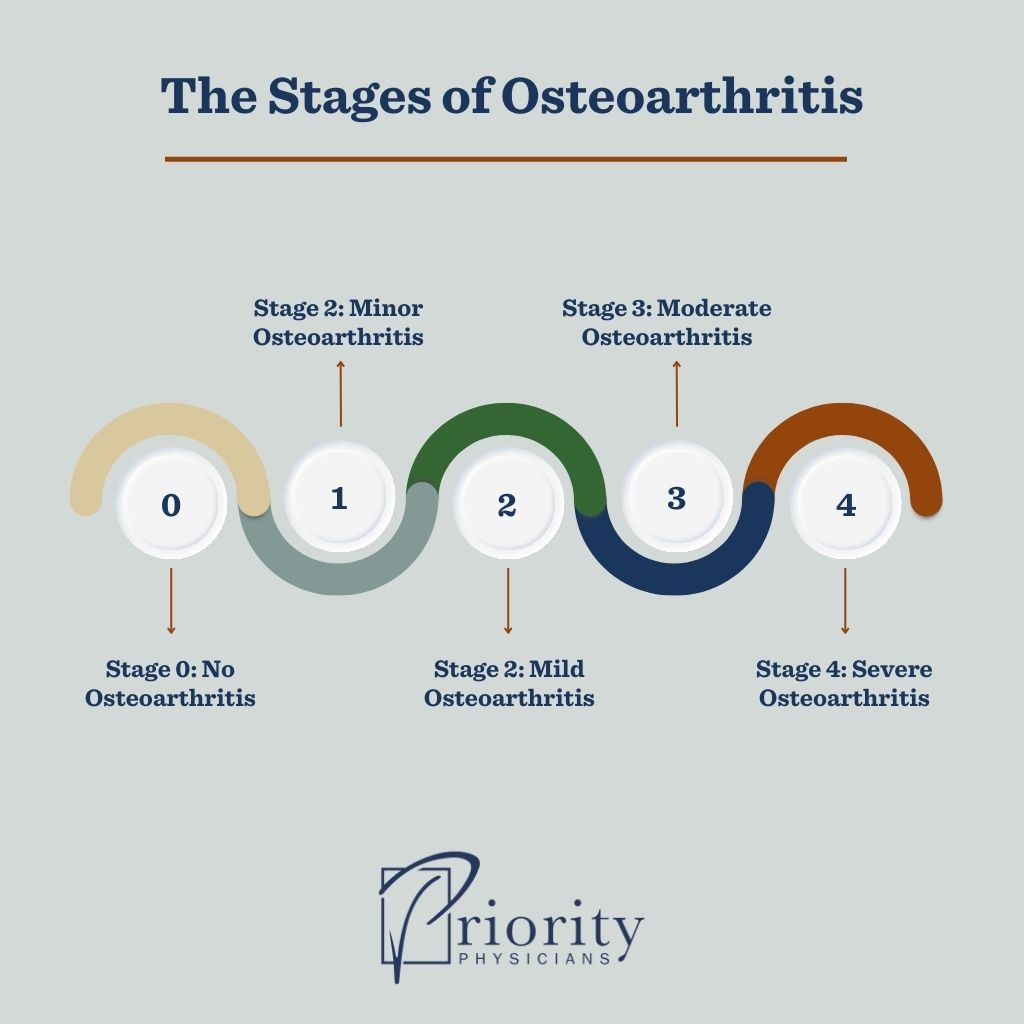
An X-ray will quickly show whether osteoarthritis is present. It will also show the stage of osteoarthritis, from 0 to 4:
- Stage 0 — no osteoarthritis
- Stage 1 — minor osteoarthritis
- Stage 2 — mild osteoarthritis
- Stage 3 — moderate osteoarthritis
- Stage 4 — severe osteoarthritis
When Should You See a Doctor About Joint Pain?
The main symptom of osteoarthritis is pain. And osteoarthritis is a progressive disease. Once you experience the first stage of pain, unless you intervene, you will eventually reach the third stage:
- Stage 1 — a predictable, sharp pain usually brought on by mechanical injury to the joint
- Stage 2 — pain becomes more common and constant, including more stiffness and affecting activities of daily living
- Stage 3 — a constant, dull, aching pain peppered with episodes of intense, exhausting pain, resulting in limited range of motion and function
If you experience second-stage pain that affects your daily activities, don’t ignore it. Instead, make time to see your doctor for a diagnosis. They can explore treatment options with you and help you take action to slow the progression of your osteoarthritis.