Family medical history can be a scary thing. Sometimes genetics can feel like a curse.
If your grandpa died of cancer, and your dad got cancer, will you get cancer?
What about a heart attack? Diabetes?
We all die from something. But many people want to know how they’re going to die so they can prevent it as long as possible. They research family medical history, assess risk, and try to figure out where the threat will come from so they can guard against it.
The Role of Genetics in Future Health
The good news is, your health outcomes are determined by more than your genetics. Your lifestyle, your environment, and even where you live all play huge roles.
So just because you have cancer in your family medical history doesn’t mean you’re destined for cancer, too.
Predisposition vs. Predestination
First, let’s talk a little about predisposition.
If you have certain genetic markers, you might be predisposed toward developing certain conditions more easily than others. But being predisposed to a health condition does not mean you’re predestined to have it. It’s not your destiny.
You have a great deal of power in managing your health. By taking control in areas like lifestyle and environment, you can significantly reduce your risk.
You can start by talking to your doctor about your family medical history. They can begin appropriate screenings for conditions you might be at risk for.
Also, if you know you’re predisposed to certain conditions, you can assess any lifestyle factors that might increase that risk. For example, if your family medical history says you’re predisposed to diabetes, you can choose to skip desserts, take more post-dinner walks, and try intermittent fasting.
In this way, your genetics and family medical history can actually help you avoid the very illnesses they predispose you toward. They’re like warning signs telling you, “Detour ahead.”
The List of Genetic Threats Is Shorter Than You Think
There are actually very few serious health conditions that are strictly hereditary. If you inherit the genes for these diseases, you will get them, regardless of lifestyle or environment.
One of the most serious is Huntington’s disease. If one of your parents had Huntington’s, you will also have it. But because of recent work in genetics, we have been able to identify all the families in the U.S. that have Huntington’s disease. No one is going to get Huntington’s disease without knowing it.
Other hereditary diseases include cystic fibrosis, Tay-Sachs disease, and sickle-cell anemia.
The Role of Lifestyle in Future Health
Heart disease, cancer, and diabetes are a very different story from these heritable diseases. Let’s look at what lifestyle can do to keep them from gaining ground.
Caution, Not Catastrophe
Your family medical history is a cautionary tale, not a death sentence. It’s where you could end up if you don’t take control of your health.
In fact, a family medical history may not even indicate a genetic predisposition.
Let’s say your dad had diabetes. You may worry that means you will, too. But if your dad weighed 400 pounds and didn’t exercise, it’s more likely lifestyle led to his condition than genetics.
Instead of believing diabetes is a foregone conclusion for you, ask yourself (and your doctor) what decisions you can make each day that will bring you a different outcome.
Lifestyle vs. Genetics
As medicine becomes more individualized, we’re learning lifestyle has a much bigger impact on health than we previously knew.
We’re just beginning to understand the mechanisms that affect whether certain genes in a person’s genetic makeup are expressed or not. So even if you do have a genetic predisposition, lifestyle can determine whether or not your body ever “sees” that gene.
This means you have control over mitigating the risks passed down through the family tree.
Advances in technology have made it easier than ever to map our genetics with something as simple as a cheek swab. Screening tools like GeneSight, which we use here in the office, examine certain genes with far-reaching health implications to give us insights that can help us make better decisions for your healthcare.
Modern medicine is allowing us to minimize the impact genetics has on our health, and building a healthy lifestyle is part of that.
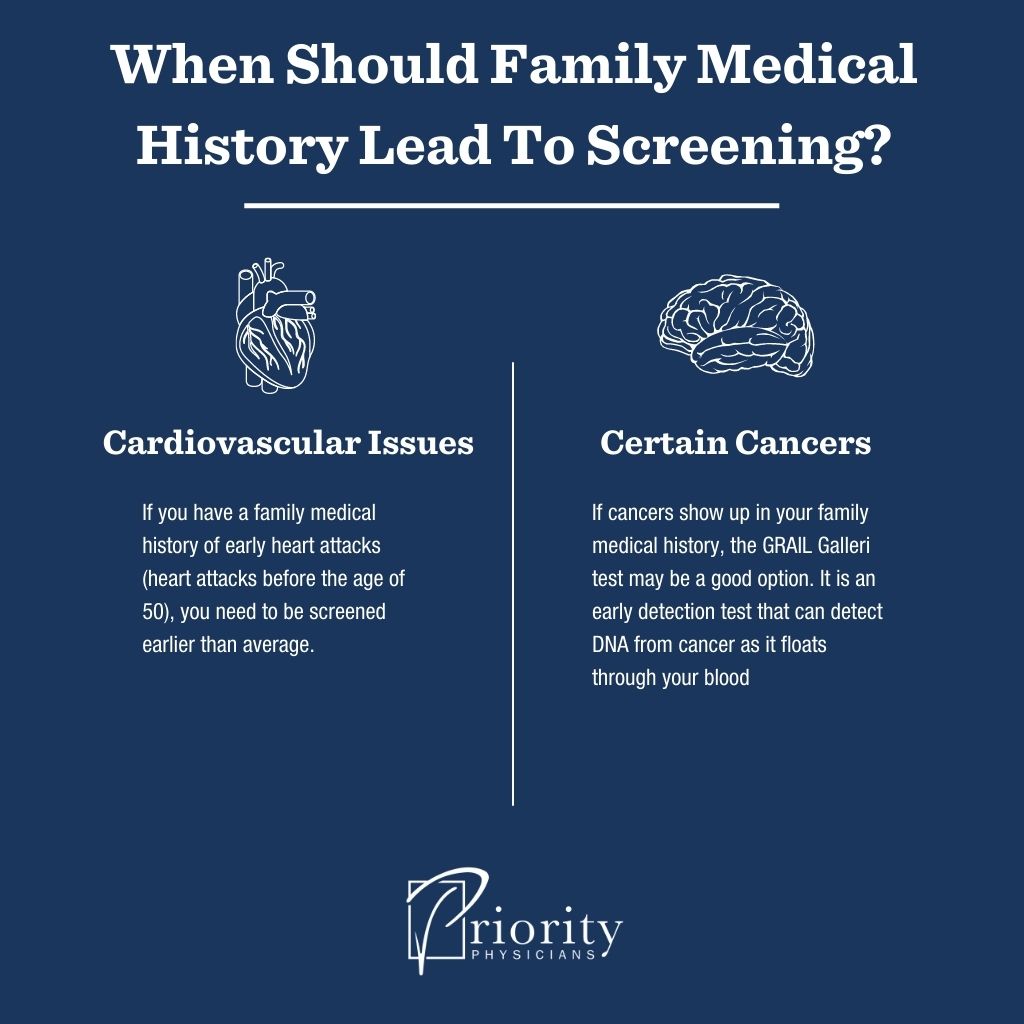
When Should Family Medical History Lead To Screening?
Cardiovascular Issues
If you have a family medical history of early heart attacks (heart attacks before the age of 50), you need to be screened earlier than average.
This looks like EKGs, cholesterol tests, apolipoprotein E genotyping, stress tests, and coronary CT angiograms. Thanks to advances in technology, tests like these are now less invasive and more efficient in evaluating cardiovascular health. You’re most likely to find some of these newer tests available with a direct primary care or concierge physician.
Certain Cancers
Physicians do a great job of screening for the five most common cancers: lung cancer, breast cancer, prostate cancer, colon cancer, and skin cancer. Fewer people die from these cancers each year because we catch them early enough to effectively treat.
More deaths are caused by the cancers that there are no standard screenings for, such as pancreatic cancer or thyroid cancer.
This is where the GRAIL Galleri test comes in.
The GRAIL Galleri test is an early detection test that can detect DNA from cancer as it floats through your blood. So while you should still go in for the standard recommended screenings for the big five, the GRAIL test can check for other forms of cancer creeping in. This simple blood test is an especially good option if these other cancers show up in your family medical history.
Mitigate Your Risk With These Best Practices
Intermittent Fasting
Mitigating your risk for certain diseases might be as simple as not eating as much. Of course, that’s easier said than done, especially living in a culture where portion sizes get bigger every year.
Intermittent fasting can help regulate insulin levels, manage weight, lower blood pressure, and stabilize hormones. It may even reduce your chance of getting certain cancers.
Try taking a long break between your last meal of the day and your first meal of the next day. You can start with a 12-hour fasting window, and then add a little more time each week until you reach 14 to 16 hours of fasting.
Exercise
Exercise is a crucial part of a healthy lifestyle. And contrary to popular belief, it doesn’t require a lot of equipment, special clothing, or an expensive gym membership.
Exercise can help regulate insulin levels, manage weight, lower blood pressure, stabilize hormones, increase bone density, strengthen the cardiovascular system, and improve mood. It might even help keep troublesome genes hidden.
Try to get at least 150 minutes of moderate-intensity aerobic activity per week. Incorporate moderate-to-high intensity muscle training at least two days per week. If you aren’t there yet, start slowly, perhaps by walking, and gradually add a little more activity every week.
Sleep
Sleep is so important. Good sleep can help lower blood pressure, stabilize hormones, improve cognitive function, and manage stress levels.
Try to get at least seven hours of sleep per night and build a bedtime ritual to follow every night. Going to sleep and waking up at around the same time every night, even on the weekends, can help.
To get started developing good sleep habits, set a timer to remind you when it’s time to unplug and wind down for the night.
Stress Management
We live in a high-stress world, and it wreaks havoc on us.
Stress causes an inflammatory response in the body, making us more prone to sickness and disease. If we don’t take control of stress, it takes control of us.
To manage your stress, cut down on clutter and distractions in the areas where you work and rest. Take breaks from technology to rest your eyes, move your body, and find ways to relax. Listen to your body when it tells you it needs rest, and when it tells you something is wrong.
Find a Direct Primary Care Physician
One of the most important tools for mitigating your risk of disease is a strong relationship with a caring physician.
If you’re concerned about your genetics or your family medical history and are ready to change your lifestyle, find a DPC or concierge physician who you can speak openly with and who will walk with you on every step of your healthcare journey.
Having a solid relationship and a high level of access to your doctor will ensure your predisposition doesn’t become your predestination.
The Final Word
Don’t let a poor family medical history determine your health outcomes. You have more control than you think. By changing your lifestyle, building healthy habits, and developing a relationship with your DPC physician, you can live a happy and healthy life

