Leukemia was once a fatal disease — in the majority of cases, at least — that largely affected children.
Now, thanks to decades of funding and research on leukemia, it’s no longer a definitive death sentence. Leukemia is now considered a chronic condition — like hypertension and diabetes — rather than a fatal one. A study from St. Jude’s even found an immunotherapy combination resulting in remission for 99% of children with a specific type of leukemia.
It’s also easier than ever to monitor for signs of leukemia. As long as you’re getting basic, routine lab work done, a meticulous doctor can identify early warning signs long before symptoms begin.
Since we’ve made such strides in treating this type of cancer, let’s explore what these developments could mean for other types of cancer.
What Is Leukemia?
While some cancers have specific causes we can point to, leukemia forms as a result of genetic mutations, usually with an unknown cause.
Leukemia can be difficult to conceptualize compared to cancers that start off localized as tumors, such as cancer of the liver or lungs. Leukemia is a cancer of the blood cells, and it develops when blood cells mutate and then reproduce.
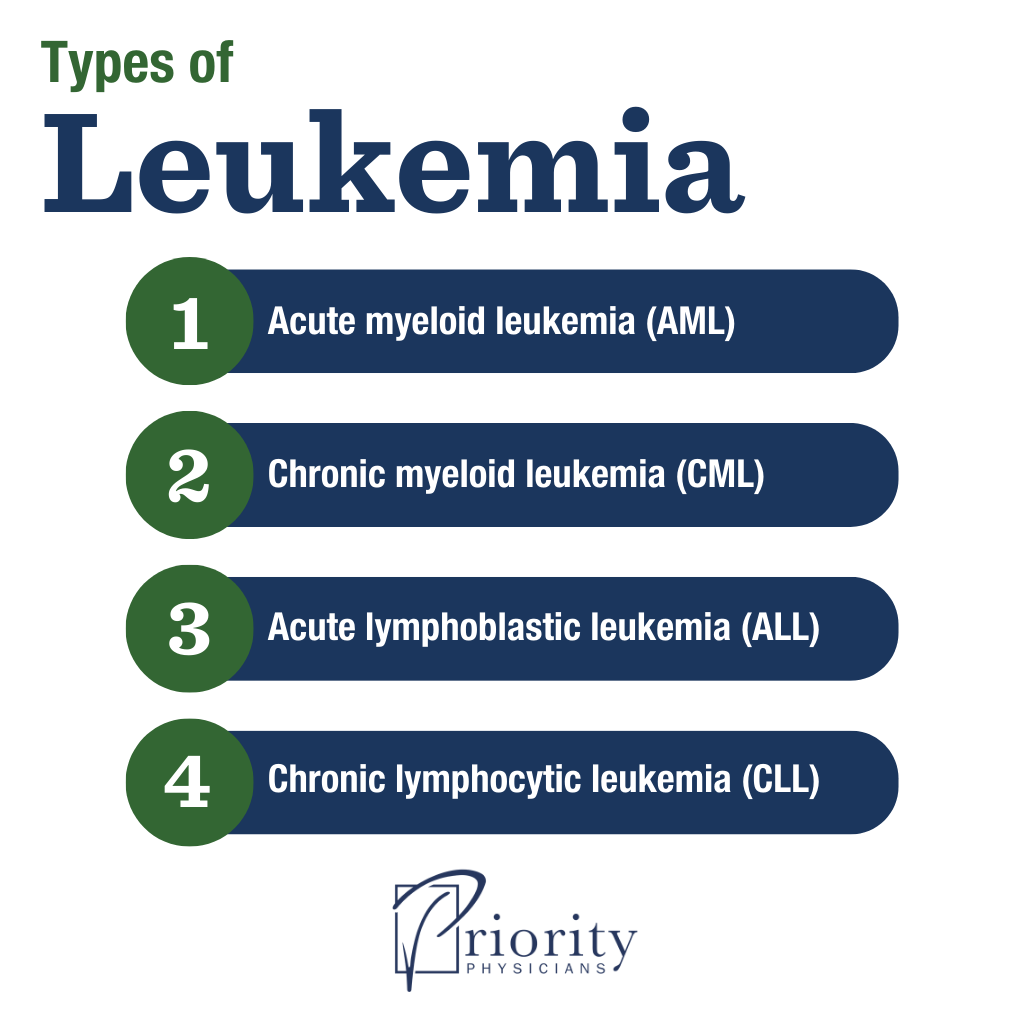
There are a few different kinds of leukemia, classified based on their speed of progression and the type of cell the cancer originates with:
- Acute myeloid leukemia (AML) is a cancer of the bone marrow, and it is the most common type of acute leukemia in adults. AML begins when unspecialized, immature blood stem cells fail to mature into normal red blood cells. Often, these stem cells instead become myeloblasts (precursors to white blood cells), and eventually result in an overproduction of abnormal white blood cells.
- Chronic myeloid leukemia (CML) is a slow-growing cancer of the bone marrow due to a genetic mutation that occurs in the chromosomes of blood cells. The mutation causes too many white blood cells to grow. These abnormal cells accumulate and eventually crowd out other crucial blood components, like platelets and red blood cells.
- Acute lymphoblastic leukemia (ALL) is a cancer of the white blood cells called lymphocytes and is the most common type of cancer in children. Blood stem cells experience a genetic mutation, producing abnormal white cells that multiply uncontrollably into billions of leukemic lymphoblasts. This reduces the number of healthy blood cells and makes disease progression incredibly fast. (We’ll discuss ALL treatment below.)
- Chronic lymphocytic leukemia (CLL) is a slow-growing cancer of the lymphocytes. The DNA of blood stem cells mutates, causing them to develop abnormal, ineffective lymphocytes that live longer and multiply more than normal lymphocytes. These cells accumulate in the body where they cause complications, such as interfering with healthy blood cell production.
Progress in Treatment: Acute Lymphoblastic Leukemia
Over the years, research on leukemia has led to more targeted treatments. For example, instead of blasting the body with constant chemotherapy and radiation, treatment for acute lymphoblastic leukemia (ALL) is now conducted in phases.
Because ALL grows rapidly, an aggressive treatment plan is standard. This process can be broken down into four parts:
1. Induction Therapy
Induction therapy is the initial phase of treatment for ALL after diagnosis. It involves destroying as many cancer cells as possible to achieve remission using a combination of medications, including corticosteroids and chemotherapy drugs. Typically, this stage requires a hospital stay of four to six weeks.
After induction therapy is complete, doctors will test a patient’s bone marrow, looking for no more than 5% lymphoblast cells. If that’s the case, then the patient is considered in remission.
However, remission doesn’t necessarily mean no abnormal cells remain. Leukemia cells too small for a microscope to detect may still remain, called “minimum residual disease” (MRD). After achieving remission, patients still need further testing for MRD since any remaining leukemia cells increase their chance for relapse. Patients may be prescribed an additional medication, the monoclonal antibody blinatumomab, if their results come back positive.
3. Postremission Treatment
Postremission treatment refers to treatments administered after a patient’s disease is in complete remission, since some leukemia cells can still remain. The goal is to prevent disease relapse.
Postremission treatment takes place in two stages:
- Consolidation, during which patients receive chemotherapy drugs at higher doses than before. Usually, doctors use a combination of several drugs to prevent leukemia cells from developing drug resistance.
- Maintenance, during which patients take chemotherapy drugs orally, at lower doses and in an outpatient setting. Side effects tend to be less severe.
4. Central Nervous System (CNS) Prophylaxis
This phase prevents leukemia cells from spreading to the area around the brain and spinal cord. CNS prophylaxis is administered throughout the entire course of treatment and consists of specific types of chemotherapy and/or radiation.
Applying Leukemia Research to Other Cancers
The phased approach that works so well with acute lymphoblastic leukemia (and a variation with acute myeloid leukemia) hasn’t yet seen as positive results when applied to other cancers. However, the approach is still an ongoing area of leukemia research and development.
It’s important to recognize the enormous potential and significance of research on leukemia. It proves diligent scientific study can improve the survivability of our most fatal diseases.
In the instance of chronic myeloid leukemia, researchers found that this previously fatal disease is the result of a chromosomal abnormality, and they developed a pill to address the particular problem that specific genetic mutation brings to the table. It’s an unbelievable breakthrough for many CML patients.
We know there are probably other cancers caused by chromosomal abnormalities as well. The discovery made with CML could help us identify those through further research — and, hopefully, apply what we know to similar kinds of treatments.
The progress the medical community has made through vigorous research on leukemia is quite encouraging. We here at Priority Physicians are hopeful about the future of cancer research and are committed to detecting early signs before it’s too late.

